Population health analytics solutions are data-driven platforms that help healthcare organizations shift from reactive care to proactive health management. These systems combine clinical records, claims data, and social determinants of health to identify at-risk patients and guide targeted interventions before problems escalate.
Key Components of Population Health Analytics Solutions:
The shift toward value-based care has made these solutions essential for healthcare organizations. As one health system found, combining clinical and claims data with social determinants helped them achieve $2.3 million in cost savings through a 9.1% reduction in per-member-per-month costs.
Modern population health platforms analyze over 4,500 clinical and social risk factors to predict outcomes like hospital readmissions, emergency department visits, and chronic disease progression. This comprehensive approach enables healthcare teams to prioritize interventions where they'll have the greatest impact on both patient outcomes and costs.
I'm Grace Ascione, a registered nurse with an MBA who has spent over 15 years helping healthcare organizations leverage data and digital marketing to improve patient outcomes and business performance. My clinical background combined with expertise in population health analytics solutions gives me unique insight into how these platforms can transform care delivery for small healthcare businesses.
Population health analytics is your healthcare crystal ball - powered by real data instead of magic. These systems help us peek into the future of patient health, spotting problems before they become expensive emergencies.
Here's what makes population health analytics different: instead of waiting for Mrs. Johnson to show up in the ER with a heart attack, we can see months ahead that she's missing her blood pressure medications and hasn't had her cholesterol checked in two years.
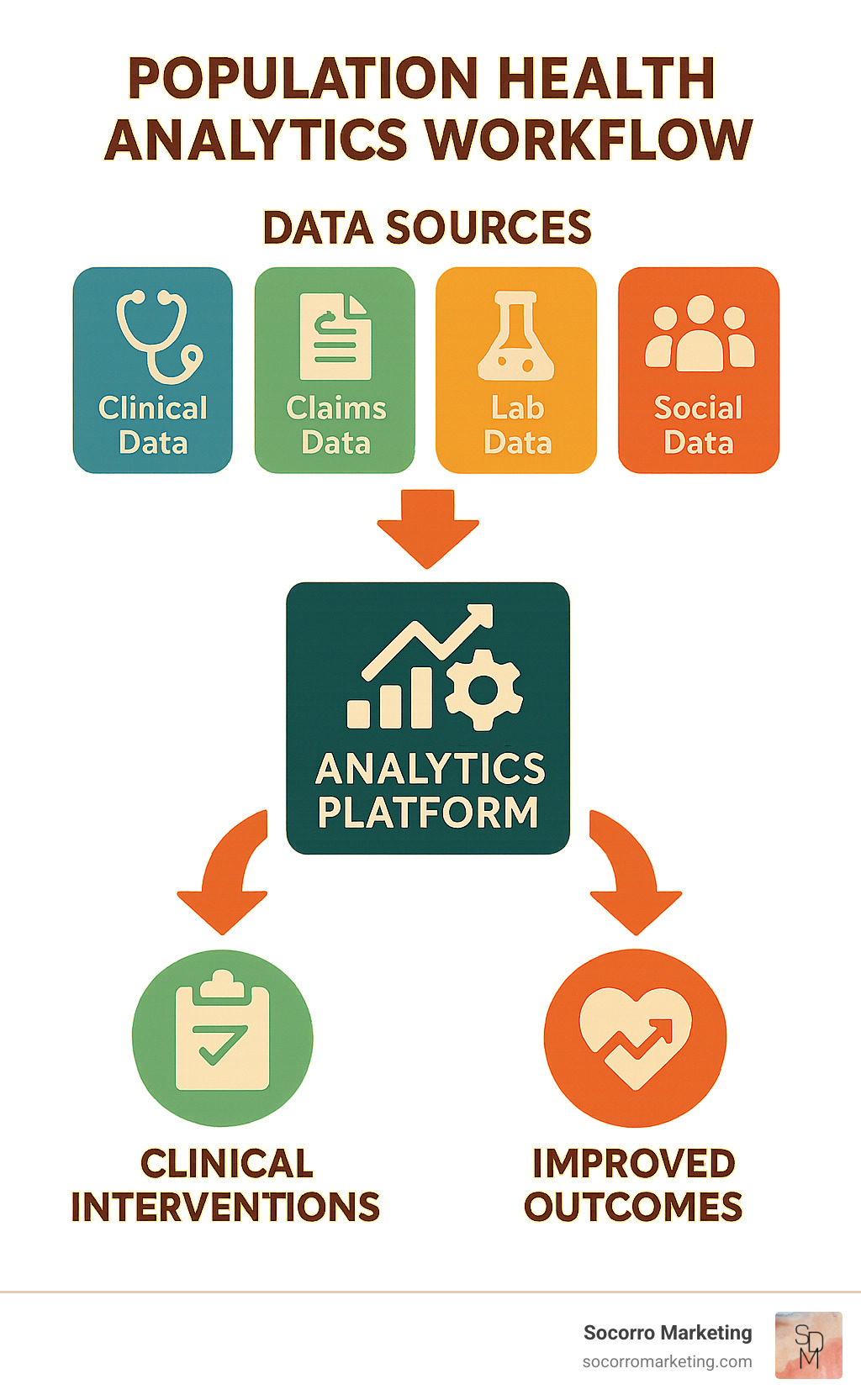
Population health analytics solutions work by gathering information from everywhere - your electronic health records, insurance claims, lab results, and even data about whether patients live in safe neighborhoods with access to healthy food.
The magic happens when we shift from reactive to proactive care. Traditional healthcare analytics might tell us that 20% of our diabetic patients ended up in the hospital last year. Population health analytics tells us which diabetic patients are most likely to end up in the hospital next year - and what we can do to prevent it.
This approach fits perfectly with value-based care models, where healthcare organizations get rewarded for keeping people healthy rather than just treating them when they're sick.
Prevention beats treatment every single time. Instead of playing healthcare whack-a-mole, these systems help us get ahead of problems. When we notice that a diabetic patient keeps missing appointments and their last A1C was creeping up, we can reach out with extra support before they end up with serious complications.
Not all patients are the same, which is why population segmentation matters so much. A 30-year-old with high blood pressure needs different care than a 70-year-old managing diabetes, heart disease, and arthritis. Smart analytics help us group patients based on their actual risks and needs.
Health equity ensures we're not accidentally making things worse for people who already face barriers to care. By looking at social factors like housing stability and transportation access, we can spot when certain groups aren't getting the care they need.
The real power of population health analytics solutions comes from bringing together all the scattered pieces of information about patients' lives.
Clinical records from electronic health systems give us the medical basics - diagnoses, medications, vital signs, and care plans. Claims data shows us the bigger picture of where patients go for care, including visits to specialists, emergency rooms, and pharmacies.
Laboratory results provide hard facts about what's happening inside patients' bodies. When we track lab values over time, we can spot trends that hint at problems brewing long before patients feel sick.
Wearable device data brings us into patients' daily lives, showing us how much they're moving, sleeping, and even tracking heart rhythms. Community and social data helps us understand the world patients live in - their housing situation, job stability, education level, and neighborhood resources.
Choosing the right population health analytics solutions can feel overwhelming. After working with dozens of healthcare organizations, I've learned that certain core capabilities make all the difference between success and frustration.
Data aggregation and normalization is about bringing all your scattered information together into one clear picture. Your platform needs to take data from your EHR, claims system, lab results, pharmacy records, and community health data, then organize it all so it actually makes sense together.
The best platforms excel at interoperability, which means they play nicely with the systems you already have. Look for solutions that support HL7 FHIR standards - these are like universal translators that help different healthcare systems communicate.
Risk stratification algorithms are where the magic happens. These systems analyze all that organized data to identify which patients are most likely to end up in the emergency room, miss important medications, or develop serious complications. The most effective platforms combine clinical risk scores with financial and social factors.
Patient engagement tools bridge the gap between identifying at-risk patients and actually reaching them. Your platform should support automated outreach through patient portals, mobile apps, text messages, and phone calls. The key is personalization.
Workflow embedding determines whether your insights actually get used. The best analytics in the world won't help if clinicians have to log into a separate system to access them. Look for platforms that integrate directly with your EHR, providing real-time alerts and decision support right where your care teams are already working.
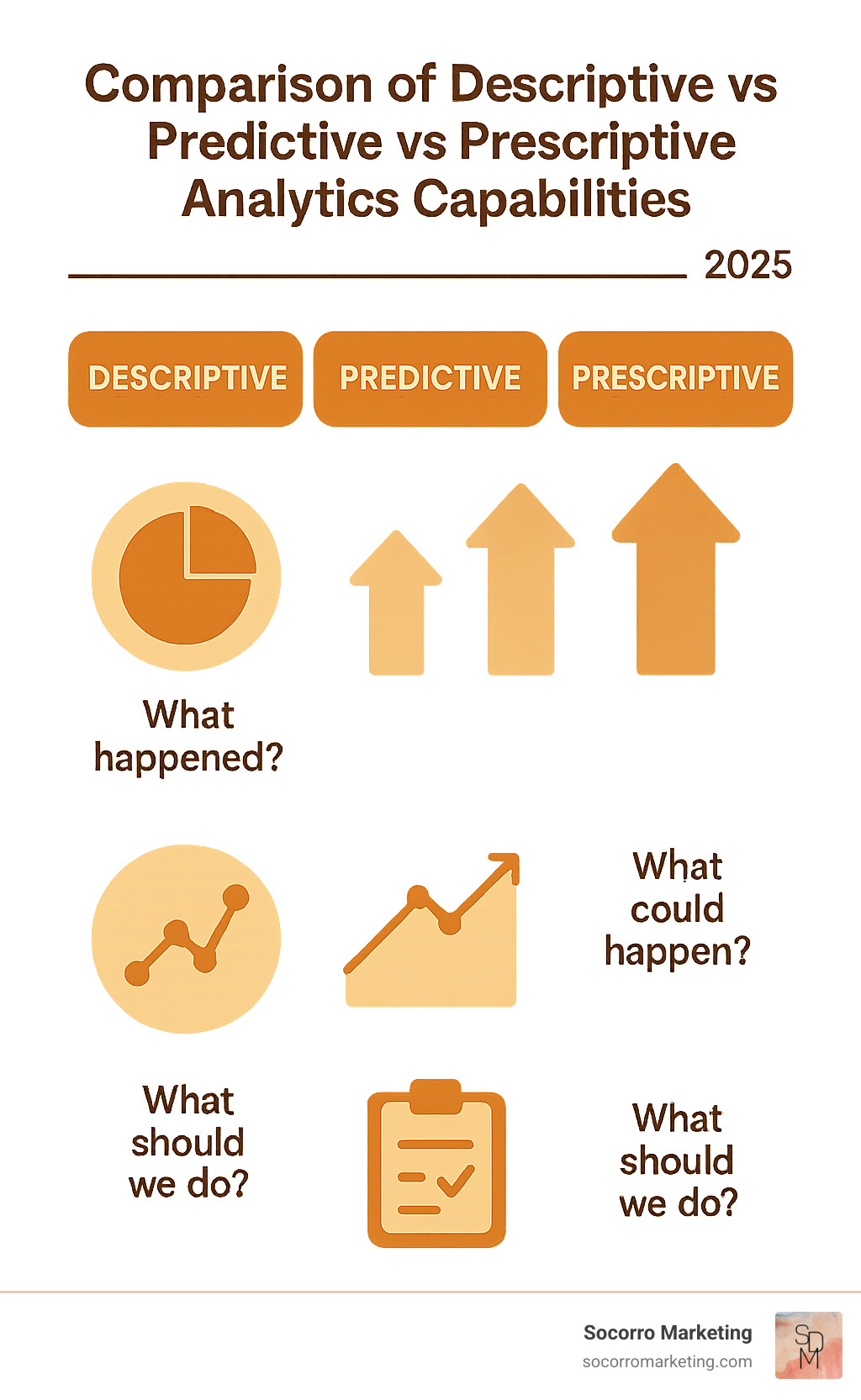
The most sophisticated population health analytics solutions go far beyond basic reporting to provide insights that can genuinely transform how you deliver care.
Machine learning and predictive modeling analyze patterns in your historical data to predict what's likely to happen next. These algorithms can identify patients at high risk for hospital readmission by examining factors like previous admissions, medication adherence, social support systems, and existing health conditions.
Prescriptive intelligence represents the next step beyond simply predicting problems. Instead of just telling you which patients are at risk, these systems recommend specific actions most likely to improve outcomes for individual patients.
Geospatial mapping helps you understand how neighborhood factors influence your patients' health outcomes. By connecting patient addresses to census data, you can identify communities with high social risk and target your outreach efforts accordingly.
Cohort builder tools allow your team to create custom patient groups based on multiple criteria. Your care managers might want to focus on diabetic patients with poor medication adherence, or your quality team might need to identify everyone due for cancer screenings.
Population health analytics solutions become absolutely essential when your organization takes on financial risk for patient outcomes. These platforms provide the insights you need to manage both quality and costs effectively in value-based care arrangements.
Cost benchmarking capabilities help you understand how your performance compares to regional and national standards. Your platform should track total cost of care, per-member-per-month expenses, and utilization patterns across different service categories.
Quality measures tracking ensures you stay compliant with regulatory requirements and contract specifications. The most comprehensive platforms support over 240 quality measures including ACO, HEDIS, and MIPS requirements.
Care gap closure tools identify patients who are missing recommended screenings, medications, or follow-up appointments. These systems should prioritize gaps based on clinical importance and individual patient risk levels, then support automated outreach to schedule needed services.
Getting population health analytics solutions up and running successfully takes more than just buying software and hoping for the best. After helping healthcare organizations across Colorado, Utah, Arizona, and New Mexico implement these systems, I've learned that the technical setup is actually the easy part - it's the people and process changes that make or break your success.
Data governance needs to be your first priority. You need clear rules about who can access what data, how to keep it accurate, and how to protect patient privacy. This means assigning specific people to be responsible for data quality and creating processes to catch errors before they mess up your analytics.
Interoperability standards are crucial for making sure your new analytics platform can actually talk to your existing systems. Work with your vendors early to ensure everything can connect properly using standards like HL7 FHIR.
HIPAA compliance becomes more complex when you're pulling data from multiple sources and creating new patient insights. You need strong security measures, careful access controls, and thorough audit trails.
Change management is where most implementations stumble. Your clinical staff already feel overwhelmed, and they're naturally suspicious of any new system that promises to make their lives easier. The key is showing them exactly how these tools will help them provide better patient care.
Just like we help healthcare organizations develop comprehensive digital marketing strategies that actually fit into their daily operations, population health analytics solutions need to align with how your organization actually works.
Data quality issues are probably the most common problem we see. If your underlying data is full of errors, incomplete records, or inconsistent coding, your analytics will be worthless. Start by implementing data validation rules that catch errors at the point of entry. Create regular data quality audits and train your staff on proper documentation practices.
Privacy and security concerns intensify when you're combining data from multiple sources. Address these concerns by implementing role-based access controls that ensure people only see data they need for their job. Use encryption for data storage and transmission. Create comprehensive audit logs that track every access and action.
Siloed systems create headaches when different departments use incompatible technologies that don't talk to each other. Work with your IT team to establish integration standards and look for platforms that offer pre-built connections to common healthcare systems.
User training and adoption often get shortchanged during implementation. Develop comprehensive training programs that focus on how the system improves daily workflows, not just which buttons to click. Provide ongoing support after go-live.
The most successful population health analytics solutions don't require clinicians to log into yet another system to find the information they need. Instead, they deliver insights directly into existing workflows where decisions are actually made.
EHR integration should feel seamless to end users. When a physician opens a patient's chart, they should automatically see risk scores, care gaps, and intervention recommendations without having to click through multiple screens.
Real-time alerts can be incredibly powerful when used thoughtfully, but they can also create alert fatigue if overdone. Configure alerts to notify care teams about truly actionable situations - like when a high-risk patient misses an important appointment or visits the emergency department.
Automated outreach capabilities let you stay connected with patients between visits based on their individual needs and preferences. This might include appointment reminders for patients who frequently no-show, medication refill notifications for those with adherence issues, or educational materials custom to specific conditions.
The most exciting part of working with population health analytics solutions is witnessing the real-world changes they create. After years of helping healthcare organizations implement these systems, I've seen how data-driven insights translate into better patient outcomes and stronger financial performance.
Cost Savings tell a compelling story. Healthcare organizations using advanced analytics platforms consistently report significant reductions in per-member-per-month costs. Some achieve over $2 million in annual savings through smarter resource allocation and proactive patient management.
The PMPM reduction of 9.1% that leading organizations achieve reflects a fundamental shift in how care is delivered. Instead of waiting for patients to get sick, these systems help healthcare teams intervene early when problems are still manageable and less expensive to treat.
Chronic Disease Prediction capabilities continue to amaze me. Research on chronic disease prediction demonstrates that modern algorithms can forecast the development of conditions like diabetes, heart disease, and COPD years before clinical symptoms appear.
Perhaps most importantly, health equity improvements occur when organizations use analytics to identify and address disparities in care. By analyzing outcomes across different demographic groups, healthcare teams can target interventions to underserved populations.
The success stories from population health analytics solutions implementations continue to inspire me. These aren't theoretical benefits - they're measurable improvements happening in real healthcare organizations.
Readmission reduction programs using predictive analytics have achieved 12-15% decreases in 30-day readmissions. These programs work by identifying high-risk patients before discharge and implementing intensive follow-up protocols.
Care gap closure initiatives have successfully closed 40% of identified gaps in preventive care within single quarters. By using analytics to identify patients overdue for screenings and implementing automated outreach programs, organizations ensure patients receive the preventive services they need.
Utilization savings of $10 million or more have been identified through analytics platforms that reveal opportunities for cost reduction. These savings come from reducing unnecessary testing, optimizing referral patterns, and managing high-cost chronic conditions more effectively.
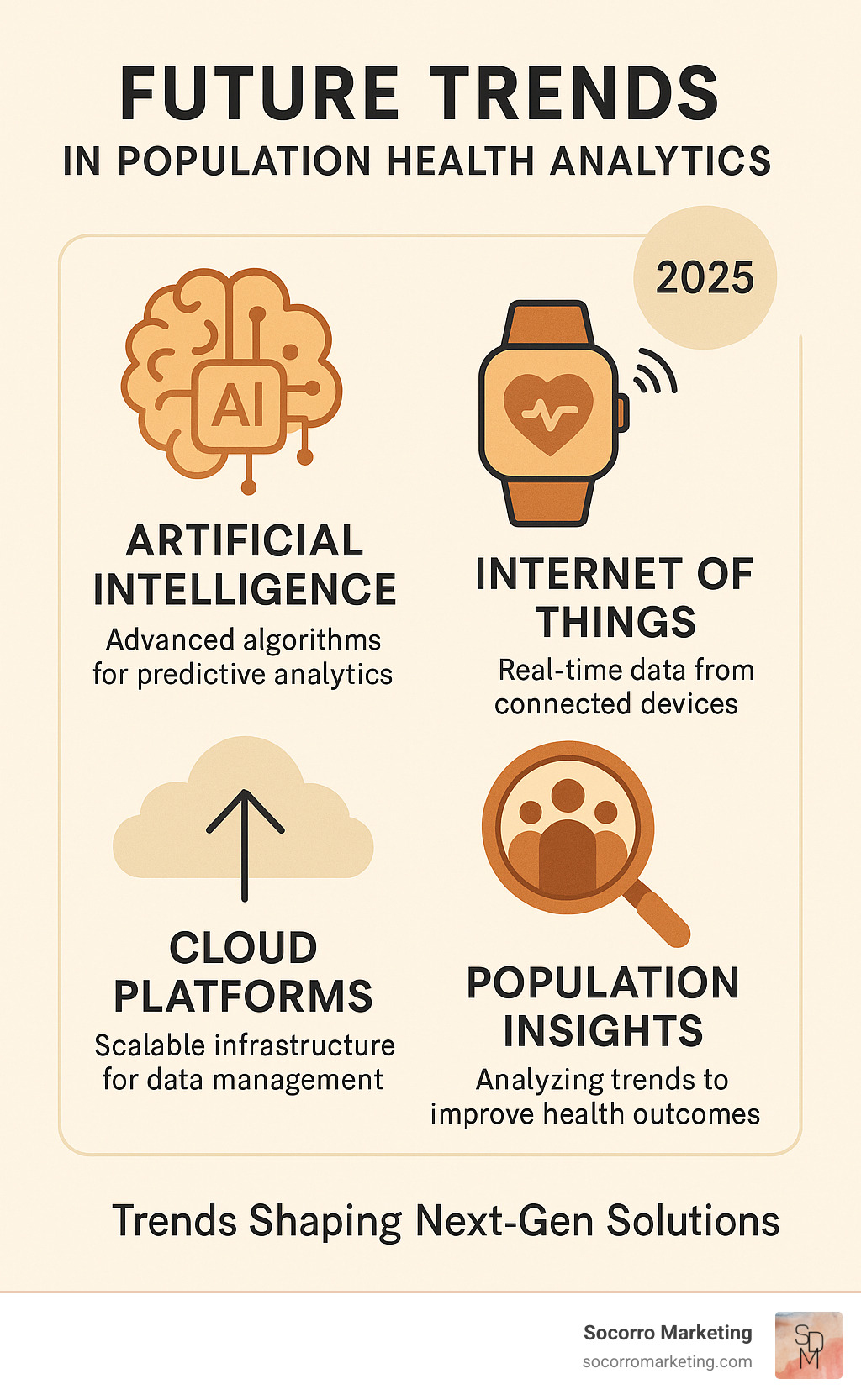
The future of population health analytics solutions excites me because emerging technologies promise even greater capabilities for improving patient care.
Artificial Intelligence and Machine Learning continue to evolve, with advanced algorithms that can identify subtle patterns in patient data and predict outcomes with increasing accuracy. Generative AI is beginning to automate the creation of patient education materials, care plans, and clinical documentation.
Internet of Things (IoT) Integration brings real-time monitoring capabilities through wearable devices and home health sensors. This continuous data stream provides unprecedented insights into patient health status between clinical visits.
Cloud-Native Platforms are becoming the standard for new implementations, offering approximately four times lower total cost of ownership compared to traditional on-premise systems. These platforms provide automatic updates, improved security, and seamless integration capabilities.
Self-Service Analytics tools are democratizing data analysis, enabling clinicians to create custom reports and analyses without waiting for IT support. This puts insights directly into the hands of the people who can act on them most effectively.
Digital Twins represent an emerging concept where virtual models of patient populations enable scenario planning and intervention testing before implementation.
Social Risk Mapping is becoming more sophisticated, with platforms able to analyze community-level factors down to the census block level. This granular view of social determinants enables targeted community interventions and resource allocation where they're needed most.
The difference between traditional healthcare analytics and population health analytics solutions is like comparing a rearview mirror to a GPS navigation system. Traditional analytics tells us where we've been, while population health analytics shows us where we're going and how to get there safely.
Traditional healthcare analytics focuses on retrospective reporting - generating monthly reports about what happened last quarter. You might see that your readmission rate was 12% or that diabetes patients had 15% more emergency visits than expected. While this information is useful, it doesn't help you prevent those problems from happening again.
Population health analytics solutions flip this approach entirely. Instead of telling you about last month's readmissions, these systems identify which patients are most likely to be readmitted next week and recommend specific actions to prevent those readmissions.
The data integration is also much broader. Traditional analytics typically pulls from one or two sources - usually your EHR and maybe billing data. Population health platforms combine clinical records with social determinants of health, community factors, and even data from patients' wearable devices.
Accurate risk stratification is like putting together a complex puzzle - you need all the pieces to see the complete picture. Population health analytics solutions excel at bringing together diverse data sources that traditionally lived in separate systems.
Clinical data from your electronic health records provides the foundation. This includes diagnoses, medications, vital signs, and care plans. But relying only on clinical data is like trying to understand a movie by watching just the final scene.
Claims data reveals the full story of how patients use healthcare services, including visits to specialists, emergency departments, and pharmacies outside your health system. This data is essential for understanding total cost of care.
Laboratory results offer objective measures that can predict problems before patients develop symptoms. Trending a diabetic patient's A1C levels over time, for example, can reveal early signs of complications months before they become clinically apparent.
Social determinants of health data might be the most important piece of the puzzle. Information about housing stability, food security, transportation access, and neighborhood characteristics helps explain why some patients struggle with their health despite receiving good clinical care.
Patient-generated data from wearable devices, patient portals, and mobile apps provides real-time insights into what's happening between clinical visits.
Measuring return on investment from population health analytics solutions requires looking beyond simple cost calculations to understand the full spectrum of benefits these platforms provide.
Direct cost savings are often the most visible and compelling. Organizations track reductions in hospital readmissions, emergency department visits, and expensive specialist referrals. Many health systems report per-member-per-month cost reductions of 5-10% within the first year.
Quality measure improvements contribute significantly to ROI, especially for organizations participating in value-based contracts. Better performance on quality metrics can result in substantial bonus payments.
Operational efficiency gains accumulate over time as staff spend less time on manual data collection and report generation. Some organizations save thousands of hours annually that can be redirected to patient care activities.
Revenue improvements come from multiple sources. Better care gap closure ensures patients receive recommended preventive services. Improved risk adjustment coding accurately reflects patient complexity. Increased patient engagement leads to higher visit volumes for preventive care.
The key to measuring ROI effectively is patience. While some benefits appear immediately, the full impact of population health programs typically takes 12-18 months to materialize.

Population health analytics solutions represent a fundamental shift in how we approach healthcare delivery, moving from reactive treatment to proactive health management. These platforms combine clinical data, claims information, and social determinants to create comprehensive patient views that enable targeted interventions and improved outcomes.
The evidence is clear: organizations implementing comprehensive population health analytics achieve significant cost savings, improved quality measures, and better patient outcomes. From $2.3 million in documented cost savings to 40% improvements in care gap closure, these solutions deliver measurable value.
Your Actionable Roadmap for Success:
Start with clear goals - Define what you want to achieve with population health analytics, whether it's reducing readmissions, improving chronic disease management, or succeeding in value-based contracts
Assess your data infrastructure - Evaluate your current EHR, claims data access, and integration capabilities to understand what technical work will be required
Choose the right platform - Select a solution that offers strong interoperability, embedded workflow integration, and advanced analytics capabilities that match your organizational needs
Plan for change management - Invest in training, communication, and ongoing support to ensure clinical staff accept and effectively use the new tools
Measure and iterate - Establish baseline metrics and regularly assess progress toward your goals, adjusting strategies based on what the data reveals
The future of healthcare depends on our ability to use data effectively to improve patient outcomes while controlling costs. Population health analytics solutions provide the foundation for this change, but success requires more than just technology - it requires a commitment to data-driven decision making and continuous improvement.
At Socorro Marketing, we understand the unique challenges healthcare organizations face when implementing new technologies and processes. Our nurse-managed approach combines clinical expertise with marketing and analytics knowledge to help healthcare businesses succeed in an increasingly complex environment. Just as we help organizations develop effective SEO strategies and keyword research to reach their target audiences, we can help you steer the complex world of population health analytics to achieve your patient care and business objectives.
The journey toward proactive, data-driven healthcare starts with a single step. Whether you're a small practice in Golden, Colorado, or a growing health system across the Southwest, the right population health analytics solution can transform how you deliver care and achieve your mission of improving patient health outcomes.